Postpartum
Postpartum care is the most neglected aspect of maternal health, yet a time of high risk for maternal mortality. "The majority of maternal deaths occur during or immediately after childbirth; ...up to half of all newborn deaths occur within the first 24 hours of life" (WHO et al., 2011c). While many women access antenatal care, much fewer women globally have access to postnatal care. For example, in Uganda, 75% of women who have had a live birth received no postnatal care. Only one in five mothers received postnatal care within the critical first two days after delivery (DHS Uganda 2006 cited in Were and Hasunira, 2010). For HIV-positive women, even fewer access postnatal care (Nassali et al., 2009).
It is critical that women living with HIV are retained in care for their own health following the birth of their child. "...Many pregnant women, even those found to be living with HIV and provided with antiretroviral drugs to prevent the vertical transmission of HIV, are not retained in care for their own health" (WHO et al., 2011a: 22). [See Treatment and Antenatal Care - Treatment] Postpartum interventions to prevent vertical transmission of HIV include protecting the health of the mother with triple therapy treatment for her own health and providing ARV treatment during pregnancy or during both pregnancy and breastfeeding to the mother solely for the purpose of reducing HIV transmission from mother to infant. Contraception counseling for women in order to space their next pregnancy or prevent an unintended pregnancy is also a critical -- though often overlooked -- component of postpartum intervention planning in PMTCT for HIV-positive women (Wilcher et al., 2008).
The benefits of ARV treatment for women living with HIV are clear. [See Treatment and Antenatal Care - Treatment] "Additionally, the systematic use of tritherapy could contribute to a reduction in expenditures for breast-milk substitutes (formula)" (Kouanda et al., 2010a: 848). ARV treatment for infants and children can also provide excellent prospects for survival into adulthood. However, without antiretroviral treatment, approximately half of children with perinatal infection die before two years of age (Newell et al., 2004 cited in Abrams, 2007). "International approaches for preventing MTCT of HIV now focus on child survival, not just HIV transmission, as the appropriate outcome to measure success of PMTCT programs. Ultimately, the goal is a live and healthy, HIV-negative child and an alive and healthy mother to care for that child" (Jackson et al., 2009: 226).
Mothers Need to Know the HIV Status of Their Infants
In order to appropriately assess what course of action to take, health providers and parents need to know the HIV status of infants, with the express permission of the mother. Yet in 54 reporting countries, only 15% of children both to mothers living with HIV were tested for HIV in the first two months of life (Zachariah et al., 2011a). Among 65 reporting countries, only 28% of infants born to mothers living with HIV received an HIV test within the first two months of life. Only 23% of HIV-exposed children in 87 reporting countries received co-trimoxazole within two months of birth in 2010 (WHO et al., 2011b). "In children younger than 18 months, ...the lack of appropriate laboratory facilities for PCR testing, the cost of assays, and the need to repeat PCRs in infants who are exposed to infected breast milk, makes it difficult to implement infant diagnosis programs..." (Kellerman and Essajee, 2010: 2). A potentially promising diagnostic is being developed and tested by PATH to detect HIV status in infants in less than 30 minutes (Boyle et al., 2012). In addition, testing the infant reveals the mother's HIV status which could expose her to stigma and discrimination. [See Reducing Stigma and Discrimination and HIV Testing and Counseling for Women] Infant serostatus can currently be reliably confirmed via PCR within 14 weeks (Havens and Mofenson, 2009). Without diagnosis and effective treatment, one-third of infants living with HIV die before the age of one and almost half die during their second year of life (WHO et al., 2011b).
Four Interventions to Reduce Postnatal Transmission
What works best to prevent postnatal transmission via breastfeeding has been the subject of much scrutiny. "Identified risk factors for transmission during breastfeeding include increased severity of maternal disease, mastitis and breast abscess, mixed infant feeding, maternal seroconversion during lactation, lower maternal CD4 cell count, and higher maternal HIV viral load" (Mmiro et al., 2009: 32).
Formula Feeding May Increase Infant Mortality Where There is No Access To Clean Water
Infant formula feeding may avert transmission of HIV via breastfeeding. However, there are more than one billion people globally without adequate access to clean water, leading to over 1.8 million child deaths from diarrhea and other diseases caused by unclean water and poor sanitation. Some have argued that advanced biomedical approaches to preventing vertical transmission "should not detract from the need for... greater access to clean drinking water and safe environment to support formula feeding" (Saloojee and Cooper, 2010: 342).
In settings prevalent in most of the developing world where there is no access to safe, clean drinking water, HIV-positive women who use infant formula may see their baby, who was born HIV-negative, die from diarrheal diseases if fed formula. "Several studies confirm that the benefits of shortening breastfeeding are offset by adverse outcomes in those infants who escape infection" (Kuhn et al., 2009a: 83). Globally, breastfeeding leads to about 300,000 HIV-positive infants every year, while at the same time, UNICEF estimates that not breastfeeding and having infants formula fed with contaminated water leads to approximately one and a half million child deaths per year (Fletcher et al., 2008). Additionally, concerns have been raised that promoting infant formula as a best practice to prevent vertical transmission may have negative consequences by decreasing breastfeeding of infants. Even in countries such as Botswana, where "almost the entire population has access to piped water..." (Creek et al., 2010: 14) and where no-cost infant formula is provided and 64% of HIV-positive women received formula following delivery, flooding in 2006 led to an outbreak of diarrheal disease, resulting in 35,046 cases and 532 deaths, 97% of these in children under the age of 2 and 64% with mothers living with HIV. "Many factors that influence the safety of replacement feeding are external to the individual household, a reality that is difficult to account for during infant feeding counseling" (Creek et al., 2010: 19). Even in higher income countries such as Botswana and South Africa, the supply of infant formula through public health facilities is unreliable (Goga et al., 2009 cited in Doherty et al., 2010).
New Guidelines About Infant Feeding Still Leave Unanswered Questions
 For women who do not have access to ARVs for either treatment or MTCT prophylaxis and who do not have access to clean water to make formula feeding safe, health providers have been advising breastfeeding. Many studies have shown that mixed feeding increases the risk of HIV transmission from the HIV-positive mother to her infant. Experts thus advise that it is better for an HIV-positive mother to exclusively breastfeed than to breastfeed and add any additional nutrition in the way of food or water prior to six months (Kuhn et al., 2009a). After six months, for HIV-positive mothers who do not have access to clean water, infant survival is increased by continued breastfeeding and adding additional nutrients for the child. Breastfeeding beyond six months, however, may increase the risk of HIV infection of the infant to 9.68% by the time the infant is two years old (Taha et al., 2007). Experts advise that infants who are HIV-positive should be breastfed. However, in most cases, the choice of feeding is often decided before the mother knows her infant's serostatus. Feeding choices can be laden with stigma as well. HIV-positive women may face heavy stigma from partners, families and communities if they formula feed their infants, yet if they do not formula feed, they may fear HIV transmission to their infants.
For women who do not have access to ARVs for either treatment or MTCT prophylaxis and who do not have access to clean water to make formula feeding safe, health providers have been advising breastfeeding. Many studies have shown that mixed feeding increases the risk of HIV transmission from the HIV-positive mother to her infant. Experts thus advise that it is better for an HIV-positive mother to exclusively breastfeed than to breastfeed and add any additional nutrition in the way of food or water prior to six months (Kuhn et al., 2009a). After six months, for HIV-positive mothers who do not have access to clean water, infant survival is increased by continued breastfeeding and adding additional nutrients for the child. Breastfeeding beyond six months, however, may increase the risk of HIV infection of the infant to 9.68% by the time the infant is two years old (Taha et al., 2007). Experts advise that infants who are HIV-positive should be breastfed. However, in most cases, the choice of feeding is often decided before the mother knows her infant's serostatus. Feeding choices can be laden with stigma as well. HIV-positive women may face heavy stigma from partners, families and communities if they formula feed their infants, yet if they do not formula feed, they may fear HIV transmission to their infants.
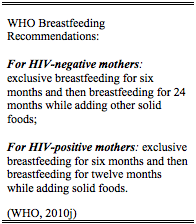
The WHO rolled out a new policy on infant feeding (whqlibdoc.who.int/publications/2010/9789241599535_eng.pdf (WHO, 2010j)), which now recommends that "mothers known to be HIV-infected (and whose infants are HIV-uninfected or of unknown HIV status) should exclusively breastfeed their infants for the first six months of life, introducing appropriate complimentary foods thereafter, and continue breastfeeding for the first 12 months of life. Breastfeeding should then only stop once a nutritionally adequate and safe diet without breastfeeding can be provided" (WHO, 2010j: 6). HIV-positive women should also know that breastfeeding does not harm their own health (Taha et al., 2006; Allen et al., 2007a; Lockman et al., 2009; Wilfert and Fowler, 2007).
The 2010 WHO guidelines state that if infant formula is given to prevent perinatal transmission, the following conditions are needed: safe water and sanitation assured at the household level and in the community; the mother or other caregiver can reliably provide sufficient infant formula milk to support normal growth and development of the infant; the mother or caregiver can prepare it cleanly and frequently enough so that it is safe and carries a low risk of diarrhea and malnutrition; the mother can, in the first six months, exclusively give infant formula milk; and the family is supportive of this practice; and the mother or caregiver can access health care that offers comprehensive child health services (WHO, 2010j: 7). In 2010, these WHO guidelines represented the best available evidence that was informed by a risk/benefit analysis of economic and other factors specific to resource-limited settings (Annexes 5 and 6; WHO, 2010j). However, this is a rapidly changing scientific landscape and it is realistic to expect best practices to change based on new evidence. In addition, these WHO recommendations will need to be tailored by countries to their specific contexts (WHO, 2010j).
The WHO also recommends that infants be given daily AZT or NVP from birth until six weeks of age (WHO, 2010j). However, the impact on future treatment options should an infant become HIV-positive while on this regimen are unclear and the infant may develop drug resistance (Zeh et al., 2011). Studies show that infant prophylaxis can decrease infant acquisition of HIV when breastfed.
Infant Feeding Research Offers Complex and Contradictory Advice
"It is confusing to us, today breastfeed, tomorrow don't." --HIV-positive mother (Chisenga et al., 2011: 155)In the absence of HAART or safe conditions for infant feeding, questions remain on how long HIV-positive women should breastfeed to minimize the risk of HIV transmission but reduce the risk of their infant dying from diarrheal disease. "How to protect the infant from complications related to non-exclusive breastfeeding and keep the child HIV free is a dilemma in the settings where replacement feeding is not safe" (Taha et al., 2011: 393). "Scientific messages... need to be clarified. Women are told both that 'Breastfeeding is a mode of HIV transmission' and 'Exclusive breastfeeding is a mode of prevention'" (Desclaux and Alfieri, 2009: 825).
WHO now recommends that women living with HIV either receive HAART while breastfeeding and beyond or to use infant formula. However, infant feeding studies have offered complex and sometimes contradictory advice on the best feeding practices and the optimal time to wean for both averting HIV transmission and reducing infant mortality (Palombi et al., 2007; Kagaayi et al., 2008; Kuhn et al., 2009c; Kuhn, 2010; Taha et al., 2007; Becquet et al., 2008; Kuhn et al., 2008; Thior et al., 2006; Leroy et al., 2008 cited in Gray and Saloojee, 2008; Becquet et al., 2007; Rollins et al., 2008). However, it is clear that for women who lack access to ARVs, the CD4 count is important in the likelihood of HIV transmission to the infant (Kuhn et al., 2009c; Kuhn, 2010). Ultimately, HAART for the mothers improves the likelihood that infants will not acquire HIV via breastfeeding (Kuhn et al., 2009c).
Studies show that mixed feeding (when a mother both breastfeeds and provides any other food, in addition to breast milk), particularly prior to the infant being four to six months of age, can put the infant at a higher risk of acquiring HIV. Studies describe the increased statistical risk of the infant acquiring HIV when mixed feeding is used, but do not describe the mechanism. It may be that the immature gut mucosa in an infant can be damaged by the introduction of other foods and nonhuman milk, thus leading to increased permeability enabling HIV viral entry (Charurat et al., 2009) or it may be that when a mother does not breastfeed regularly she can develop mastitis, a painful inflammation of the breast. Mastitis may not always be severe enough to compel a woman to receive medical care, however, studies have shown that HIV-positive women with even subclinical cases of mastitis have a higher viral load in the breast milk of the affected breast (Nussenblatt et al., 2006; Kasonka et al., 2006; Kantarci et al., 2007). Further research is needed.
Women Face Difficult Decisions in Infant Feeding
Mothers report that they struggle to stop breastfeeding at 12 months, which goes against cultural norms and could reveal their HIV-positive serostatus as well as the status of their infants, referred to pejoratively by others as "nevirapine babies." Many mothers also struggle to purchase nutritious food for their infants starting at six months (Ostergaard and Bula, 2010). Mothers living with HIV in resource-limited settings are faced with a terrible dilemma at the time of infant feeding, forced to choose between "two competing risks: exposure to malnutrition or exposure to HIV infection" (Cames et al., 2010b: 784). With infants more likely to die from malnutrition than HIV, WHO has recommended breastfeeding. Yet, HIV-positive mothers in resource-poor settings may be so motivated to protect their infant from vertical transmission, that they may stop breastfeeding early even when lacking adequate replacement foods (Lumney et al., 2008 cited in Cames et al., 2010b). In sub-Saharan Africa, breastfeeding is universal and continued until age 24 months in most settings (DHS, 2007 cited in Taha, 2011).
Women who follow WHO's current advice to breastfeed were made to feel in earlier years that if they breastfed their infants they were failing to ensure their infants survival, or worse, providers accused women of killing their infants with their breastmilk (Chisenga et al., 2011; Ostergaard and Bula, 2010). One HIV-positive mother of five in Cameroon said that she was told: "Your child is going to die if you breastfeed. You'll contaminate him" (Desclaux and Alfieri, 2009: 824). Women reported that when they breastfed, "I felt like I was giving poison to my child" (Woman living with HIV in Malawi; Ostergaard and Bula, 2010: 217). WHO's current advice presents a huge advantage as the recommendation to exclusively breastfeed for six months and then partially breastfeed for the infants' first 12 months more closely mirrors the usual infant feeding practices and will not "advertise the woman's HIV-positive status, thus reducing stigma" (Chisenga et al., 2011: 157). But women still struggle with the knowledge that breastmilk can increase the risk of HIV transmission and "are aware of the fact that the child could be given infant formula exclusively (instead of mother's milk) but as the financial cost is high, they feel too poor to buy it" (Ostergaard and Bula, 2010: 217). And some women living with HIV cannot breastfeed for the same reasons as for HIV-negative women, or as one woman living with HIV put it: "I had to leave breastfeeding because I wanted to go and look for a job" (Morgan et al., 2010: 869). "To maximize HIV-free survival among HIV-negative infants born to HIV-positive women, infant feeding recommendations must balance the risks of HIV acquisition through breast-feeding with the setting specific risks of diarrhea, pneumonia, malnutrition and death associated with replacement feeding" (Ciaranello et al., 2012). Women living with HIV also face pressures from their partners, families and communities to breastfeed for more than 12 months and to provide mixed feeding prior to the recommended six months of exclusive breastfeeding (Msellati, 2009; Gewa et al., 2011; Wachira et al., 2009; Tomasoni et al., 2011).
In many countries, formula feeding is associated with HIV and women who formula feed face stigma. For example, in Botswana, free ARVs and infant formula are widely available, as is safe drinking water; yet, more than half of women in a study did not formula feed their babies due to stigma (Shapiro et al., 2003). PMTCT programs may also inadvertently increase stigma against women living with HIV by having separate HIV facilities, home visits for HIV-positive women, or providing infant formula (Thorsen et al., 2008). For women living with HIV who have infants who are HIV-positive, breastfeeding is best, but women are often unable to know their infant's serostatus prior to deciding whether to breastfeed or not. Since the infant feeding advice that women get is contradictory, it is not surprising to find studies where "the majorities of the mothers... seemed confused about how HIV-infected mothers should feed their infants" (Falnes et al., 2010: 10). Other studies found that mothers understood the dangers of HIV transmission but that exclusive breastfeeding and exclusive replacement feeding were difficult to maintain because of the stigma of going against cultural norms and the fear that disclosing their HIV positive serostatus would lead to abandonment by their husbands, with dire economic consequences for them and their children (Chisenga et al., 2011; Fadnes et al., 2010; Ostergaard and Bula, 2010). [See Reducing Stigma and Discrimination]
Prevention of Vertical Transmission in the Postpartum Period Remains Challenging
Further research is urgently needed to clarify what works best in infant feeding in settings where infant diarrheal deaths are common to prevent perinatal transmission. "Prevention of mother-to-child HIV transmission during breastfeeding remains one of the greatest challenges facing scientists, clinicians and women in the developing world... While awaiting further studies... promoting exclusive breastfeeding with safer weaning and assuring ART for pregnant and postpartum women with advanced HIV will likely prevent the majority of needless maternal and infant deaths" (Kuhn et al., 2009a: 90-91).
Although only about half of infected infants survive their first two years without antiretroviral treatment, about a quarter will live ten years or more. As these perinatally infected HIV-positive children become adolescents will need testing, treatment and sexual and reproductive health services (Ferrand et al., 2011). [See Prevention and Services for Adolescents and Young People]
"It is easy to get overwhelmed by the enormity of the world-wide perinatal HIV epidemic and the extent of resource and infrastructure needs; however, this cannot be an excuse for inaction. Implementation will be challenging. However, the cost of indecision and delay in program implementation is high, because every pediatric HIV infection that is not prevented increases the ultimate economic and social cost to each family, community, and country" (Mofenson, 2010b: S144).


